You know the drill. The alarm goes off, and instead of feeling refreshed, you're hit with a wave of exhaustion that coffee can't seem to touch. Your partner nudges you (again) about your thunderous snoring. Maybe you've even jolted awake a few times, gasping for air. If this sounds familiar, you're not just a "bad sleeper." You might be one of the millions dealing with sleep apnea, a condition where your breathing repeatedly stops and starts during sleep. The scary part? Most people with it don't know they have it. They just think they're tired all the time.
Let's cut through the noise. This isn't another generic list of symptoms. We're going deep into what sleep apnea actually feels like, the real-world pros and cons of every major treatment, and the subtle mistakes people make that keep them from getting better sleep. I've spent over a decade talking to patients and specialists, and the gap between textbook knowledge and lived experience is wider than you think.
What You'll Find in This Guide
The Symptoms You're Probably Missing (It's Not Just Snoring)
Everyone talks about loud snoring. It's the classic sign. But focusing only on that is like diagnosing a car problem by only listening to the radio. Sleep apnea's symptoms are sneakier, often masquerading as other issues.
The daytime giveaways are huge. Do you have crushing fatigue no matter how long you're in bed? That's not normal. Morning headaches, a dry mouth that feels like sandpaper, and a foggy brain that makes focusing a struggle are huge red flags. I've had patients blame their poor performance at work on stress or aging, when it was literally their brain being starved of oxygen hundreds of times a night.
Then there's the mood stuff. Irritability, short temper, feeling depressed—these aren't just personality quirks. They're common consequences of chronically fragmented sleep. Your partner might notice the breathing pauses more than you do. They hear the snoring stop dead, followed by a loud snort or gasp as your body forces itself to breathe again. It's terrifying to witness.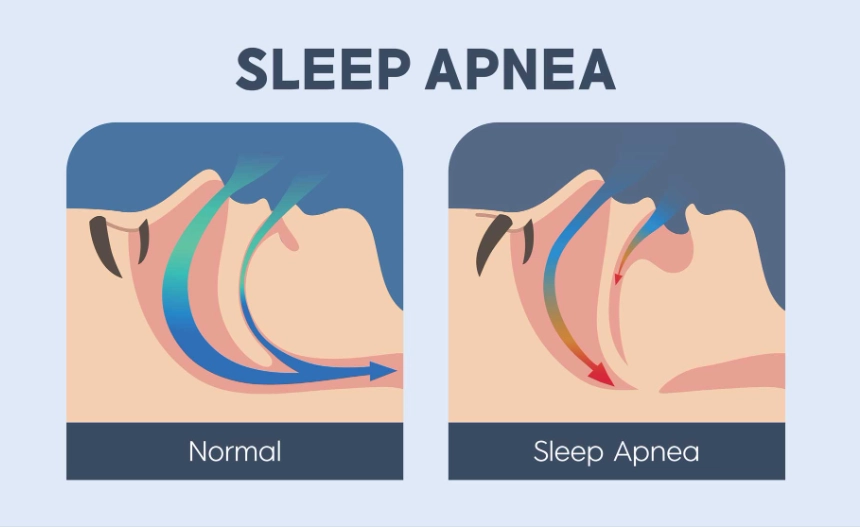
A Quick Symptom Checklist
If you check two or more of these, it's time to talk to a doctor:
- Loud, chronic snoring interrupted by silence.
- Waking up gasping or choking.
- Unrefreshing sleep, no matter the duration.
- Excessive daytime sleepiness (falling asleep at your desk, while driving).
- Morning headaches and dry mouth.
- Difficulty concentrating and memory issues.
- Mood swings, irritability, or depression.
Obstructive vs. Central: Knowing the Difference Matters
Most people have Obstructive Sleep Apnea (OSA). It's a physical problem. The muscles in the back of your throat relax too much, collapsing the airway. Your chest and diaphragm keep trying to breathe, but the air can't get through.
Central Sleep Apnea (CSA) is less common but trickier. Here, the airway is open, but your brain fails to send the proper signals to your breathing muscles. It's a communication breakdown in your central nervous system. CSA is often linked to heart failure, stroke, or opioid use. The treatment paths for these two are different, which is why a proper diagnosis is non-negotiable.
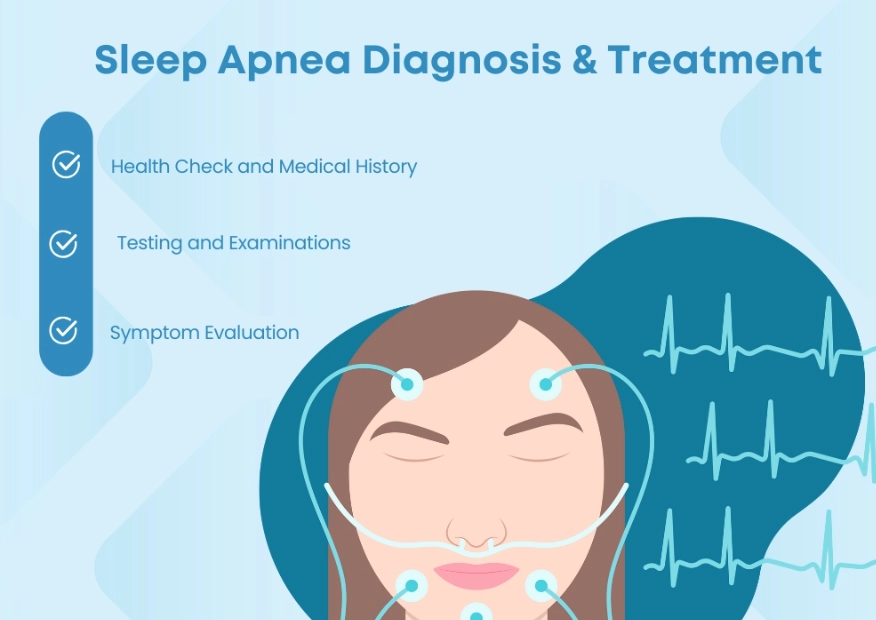
How to Get Diagnosed: From Home Tests to Sleep Labs
You can't treat what you haven't measured. The gold standard is an in-lab polysomnogram. You spend a night in a sleep clinic hooked up to wires that monitor your brain waves, oxygen levels, heart rate, breathing, and leg movements. It's comprehensive, but it can be expensive and, let's be honest, sleeping in a strange bed with wires glued to you isn't exactly natural.
The good news? For many suspected cases of OSA, home sleep apnea tests (HSAT) are a valid and convenient first step. These are simplified devices you use in your own bed. They typically measure airflow, breathing effort, and blood oxygen. They're not as detailed as the in-lab study, but they're great for catching moderate to severe OSA. The American Academy of Sleep Medicine has guidelines on who is a good candidate for an HSAT.
The key number that comes from these tests is the Apnea-Hypopnea Index (AHI). It counts how many breathing events (full pauses or shallow breaths) you have per hour of sleep.
| AHI Score (Events per hour) | Severity Level | What It Typically Means |
|---|---|---|
| Less than 5 | Normal | No significant sleep apnea. |
| 5 - 14 | Mild | May cause daytime sleepiness. Lifestyle changes often recommended first. |
| 15 - 29 | Moderate | Significant disruption. Treatment strongly advised to prevent health complications. |
| 30 or more | Severe | Major health risk. Treatment is urgent to protect heart and brain health. |
Don't get hung up on the exact number. A score of 10 with terrible daytime symptoms is more urgent than a score of 20 in someone who feels okay. The symptoms guide the treatment as much as the AHI.
A Deep Dive into Every Major Treatment Option
Treatment isn't one-size-fits-all. It's a toolkit. Your job, with your doctor, is to find the right tool for your life and severity.
1. CPAP Therapy: The Gold Standard (With Caveats)
Continuous Positive Airway Pressure (CPAP) is the most effective treatment for moderate to severe OSA. A small machine delivers a gentle stream of pressurized air through a mask, acting as a pneumatic splint to keep your airway open.
Here's the truth they don't always tell you upfront: CPAP has a high initial failure rate because of poor setup and support. The machine itself is just a blower. The magic is in the mask fitting and pressure titration. A mask that leaks or feels like a medieval torture device will end up in your closet. You need a respiratory therapist or a dedicated DME (Durable Medical Equipment) provider who will work with you to try different styles—nasal pillows, nasal masks, full face masks—until one feels tolerable.
Modern machines are quiet and smart. They have humidifiers to prevent dry nose, and they automatically adjust pressure (APAP) throughout the night. But they're not cheap, and insurance coverage can be a maze. The U.S. Food and Drug Administration (FDA) clears these devices as medical equipment, which speaks to their importance.
A friend of mine, Mark, gave up on his CPAP three times. The first mask was huge. The pressure felt like he was fighting a hurricane. On his third try, with a different specialist, he got a minimal nasal pillow mask and a machine with a "ramp" feature that starts pressure low. Now he says he can't sleep without it. The difference was night and day—literally.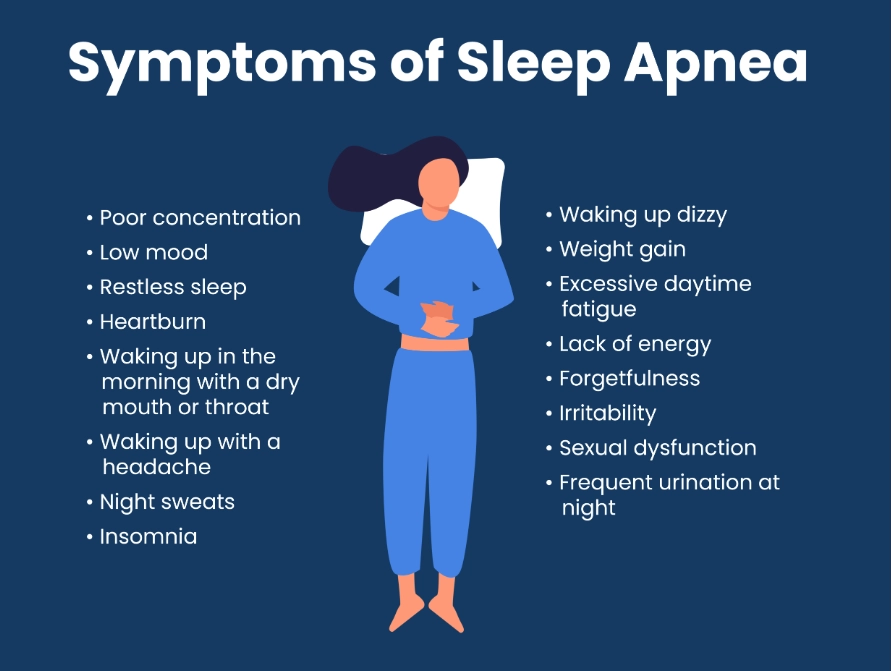
2. Oral Appliance Therapy: The Dental Approach
Think of this as a custom-fit mouthguard that gently shifts your lower jaw forward. This pulls the tongue and soft tissues away from the airway. It's prescribed by a dentist with special training in sleep medicine.
Best for: People with mild to moderate OSA, those who are CPAP-intolerant, or side sleepers. It's quiet, portable, and doesn't need electricity.
The drawbacks: It's not as effective as CPAP for severe cases. It can cause jaw pain, tooth movement, or changes in your bite over time. You need follow-ups with your dentist to adjust it and monitor for side effects. It's also an out-of-pocket expense for many, as dental insurance often doesn't cover it for sleep apnea.
3. Positional Therapy: For Position-Dependent Apnea
This is the most underrated fix. If your apnea events happen primarily when you're on your back (supine), simply training yourself to sleep on your side can work wonders. It uses gravity to keep your airway open.
You can try the old tennis ball trick (sew a sock with a tennis ball to the back of your pajamas), but dedicated devices are better. Wearable devices vibrate when you roll onto your back. Special pillows can encourage side-sleeping. For some, this simple change reduces events by 50% or more. It's a low-cost, zero-risk strategy to try immediately, even while pursuing other treatments.
4. Surgery: The Last Resort (Usually)
Surgery aims to physically enlarge or stabilize the airway. Procedures range from removing tonsils and adenoids (common in children) to more complex surgeries like Uvulopalatopharyngoplasty (UPPP) or maxillomandibular advancement (MMA).
My take: Surgery should rarely be the first option. It's invasive, recovery can be painful, and success rates are variable. It's most appropriate when there's a clear, fixable anatomical obstruction (like enormous tonsils) that other therapies can't bypass. Get multiple opinions from ENT surgeons who specialize in sleep.
Lifestyle Changes That Actually Move the Needle
Don't underestimate these. For mild apnea, they can be the primary treatment. For everyone else, they make other therapies work better.
Weight loss: Even a 10% reduction in body weight can significantly improve AHI. Excess weight, especially around the neck, puts direct pressure on the airway.
Avoid alcohol and sedatives: They relax your throat muscles even more, making collapse easier. That nightcap is making your apnea worse.
Nasal congestion management: If you can't breathe through your nose, you'll mouth-breathe, which worsens snoring and apnea. Saline sprays, nasal steroid sprays (like Flonase), or even nasal dilator strips can help. Treat allergies aggressively.
Exercise: Regular exercise, even without weight loss, can improve sleep apnea severity. It strengthens the muscles around the airway and improves overall respiratory control.
Your Sleep Apnea Questions, Answered
I snore loudly but don't feel tired during the day. Do I still need treatment?
Possibly. "Silent" sleep apnea is a thing. The lack of daytime sleepiness doesn't mean your body isn't under stress. Those repeated oxygen drops and adrenaline surges strain your cardiovascular system, increasing your long-term risk for high blood pressure, heart attack, stroke, and type 2 diabetes. A sleep study is the only way to know for sure what's happening in your body at night.
My CPAP machine is so loud and uncomfortable. How can anyone sleep with it?
You're likely using the wrong mask or settings, or you have a very old machine. Newer CPAP/APAP machines are remarkably quiet—often quieter than a whisper. The discomfort is almost always mask-related. Go back to your equipment provider and demand a mask fitting session. Try a different style. Nasal pillows are a game-changer for many because they're so minimal. Also, use the ramp feature and ensure the humidifier is correctly filled and adjusted. A well-set-up CPAP should be a gentle breeze, not a storm.
Are over-the-counter "anti-snoring" mouthpieces a good alternative to a dental appliance?
No, and this is a critical distinction. OTC boil-and-bite devices are for simple snoring. They are not designed or tested to treat sleep apnea, which is a serious medical condition. They can be dangerous if they worsen an underlying apnea by pushing the jaw into a bad position. A professionally made oral appliance is custom-fabricated from dental impressions and titrated under a dentist's supervision to ensure it opens your airway effectively and safely.
Can sleep apnea be cured, or is it a lifelong management thing?
For most adults with OSA, it's a chronic condition that requires long-term management, like high blood pressure. However, the right treatment effectively controls it. In some specific cases, a significant, sustained weight loss can "cure" it if the excess tissue causing the obstruction is gone. For positional apnea, side-sleeping can be a permanent fix. For central sleep apnea linked to another condition (like heart failure), treating the primary condition may resolve the apnea. The goal is effective control to eliminate the health risks and restore quality sleep.
 The journey to treating sleep apnea isn't always a straight line. It requires patience and partnership with the right healthcare team. But the payoff—waking up feeling alive, having energy for your family, and protecting your long-term health—is absolutely worth the effort. Start by paying attention to those subtle symptoms and having that first conversation with your doctor.
The journey to treating sleep apnea isn't always a straight line. It requires patience and partnership with the right healthcare team. But the payoff—waking up feeling alive, having energy for your family, and protecting your long-term health—is absolutely worth the effort. Start by paying attention to those subtle symptoms and having that first conversation with your doctor.




























Join the Conversation